Home » Radiology Centre Setup Guide Australia
How to set up a radiology centre in Australia: Radiology Centre Setup Guide
Setting up a radiology centre in Australia is one of the most complex healthcare projects you can undertake. It combines heavy infrastructure, strict compliance, cutting-edge IT, and multimillion-dollar imaging equipment. Every step must meet regulatory, clinical, and business standards.
This guide walks through all aspects from location and design to modalities, reporting stations, IT infrastructure, compliance, staffing, and long-term operations. It shows how Medic Cloud manages the process end-to-end, ensuring your centre launches smoothly, safely, and profitably.
🔈 Listen as podcast
Title: Radiology Centre Setup Guide AustraliaDuration: 04:47
1. Navigating the regulatory framework
A radiology centre cannot operate without satisfying multiple regulators. This isn’t an afterthought it’s the first step you need to consider according to our Radiology Centre Setup Guide.
ARPANSA RPS-19 defines radiation safety in Australia. Before you build, a shielding plan must be drawn up by an accredited medical physicist. This plan specifies wall thicknesses, protective barriers, and room orientation. ARPANSA must sign off before construction proceeds. Failing to comply can mean tearing down completed works at great cost.
Every imaging device must be approved by the Therapeutic Goods Administration (TGA). Registration is via GMDN codes, covering everything from CT scanners to ultrasound units. If you buy an imported system that isn’t TGA-approved, you risk penalties and, more critically, the loss of Medicare billing rights. We’ve covered this risk in detail in The Risks of Importing Unapproved Medical Devices into Australia.
Reporting environments must meet the standards set by the Royal Australian and New Zealand College of Radiologists (RANZCR). That means diagnostic monitors of a specific resolution and luminance, with calibration processes in place. A radiology centre that skips these requirements cannot achieve accreditation. See our blog Do I Need a Medical Grade Monitor for Radiology Reporting? for the technical detail.
Finally, data handling is governed by the Privacy Act 1988 and state legislation such as the Health Records Act 2001 (VIC). Patient images and reports must be stored on Australian servers or certified Australian cloud services. Breaches bring legal action and reputational damage.
Overlaying all this is the Diagnostic Imaging Accreditation Scheme (DIAS). Without DIAS accreditation, you cannot bill Medicare. Accreditation audits every part of the centre: quality systems, staff licensing, and radiation safety.
2. Site selection and facility fit-out
A radiology centre is only as strong as its location and design. Site selection blends clinical demand with business sense.
Look first at demographics. Older populations drive higher utilisation of CT, ultrasound, and DEXA. Areas with growing families push demand for obstetric ultrasound and paediatric X-ray. Proximity to GP clinics and specialists ensures steady referrals. Parking and disability access are non-negotiable. A centre that frustrates patients with poor access quickly loses its referral base.
Inside the facility, room sizing is critical. CT rooms require large floor areas, space for injectors and emergency trolleys, and reinforced flooring to support the gantry. X-ray rooms demand shielding thickness to ARPANSA standards. Ultrasound rooms may be smaller, but need privacy, soundproofing, and good ergonomics for sonographers.
Workflow design dictates efficiency. A patient’s path should flow seamlessly from reception, to waiting and changing areas, to imaging rooms, and finally back out. Staff corridors must be separate to reduce delays and maintain infection control. Poor layouts cost time, frustrate staff, and reduce throughput.
Facility systems underpin reliability. HVAC redundancy keeps CT rooms cool even if one system fails. UPS systems protect servers and reporting stations during power fluctuations. Electrical load must be sized not just for today’s modalities but for future expansion a centre should never have to shut down to re-wire.
Safety is equally important. OH&S standards require ergonomic controls, safe patient transfer pathways, and infection control procedures. Regulators look at these as closely as clinical systems.
3. IT and network infrastructure
Radiology today is an IT business. Without stable networks and servers, images cannot move and reports cannot be issued.
At the foundation is structured cabling. Networks must be segmented into secure VLANs: modalities, PACS servers, admin workstations, and internet access all isolated. This not only improves performance but reduces the blast radius of any cyberattack.
Redundant internet is essential. A dual provider setup fibre NBN plus 4G/5G backup ensures radiologists and referrers stay connected even when one carrier goes down. Referrers expect same-day reporting. Connectivity failures damage reputation immediately.
While cloud is popular in general business IT, in radiology on-premises servers remain essential. DICOM studies are large; CT and CBCT datasets can be multiple gigabytes. Local servers provide low latency, guaranteed performance, and sovereignty. Cloud can still play a role in long-term archiving or disaster recovery, but PACS and RIS should remain local.
Cybersecurity must be rigorous. Healthcare is the number one target for Australian cyberattacks. A radiology IT stack must include managed endpoint detection and response (EDR), strict role-based access, regular patching, and external penetration tests. Backup systems must store data in Australia to meet the Privacy Act.
For more depth, see What is a Medical-Grade Network? and our Radiology IT page.
4. Imaging modalities
A new centre must carefully choose its modalities. The mix determines patient volume, referral patterns, and ROI.
The starter pack for viability includes:
- X-ray, the backbone of diagnostic imaging.
- DEXA, vital for bone density and metabolic assessment.
- Ultrasound, versatile across obstetrics, vascular, and musculoskeletal.
- CT, essential cross-sectional imaging, though capital intensive.
- CBCT, increasingly valuable for dental, ENT, and orthopaedic work.
From there, centres can expand. Mammography supports breast screening. OPG with CEPH supports dental and orthodontic practices. Advanced centres may invest in MRI or PET, depending on market size and referral networks.
For technology trends, see DRGEM X-ray Machine Innovation and our Dental X-Ray System Guide.
5. Radiologist Reporting Environments
A radiologist’s workstation is more than a desk with monitors. It is the clinical heart of the centre.
RANZCR requires diagnostic monitors of specific resolution and luminance, calibrated regularly with audit logs. Without compliance, accreditation fails. Radiologists also need dual or triple monitor setups for RIS, PACS, and clinical tools.
Ergonomics are crucial. Rooms must be designed with low-glare lighting, acoustic control, and adjustable seating. Fatigue is a real risk in radiology; poor environments increase error rates.
Connectivity must be secure and fast. RIS/PACS must be accessible for both in-centre and remote radiologists. Many practices now include teleradiology setups to cover after-hours.
We’ve explained the requirements in our article Do I Need a Medical Grade Monitor for Radiology Reporting?.
6. Workflow and System Integration
A radiology centre lives and dies by workflow efficiency. RIS and PACS integration must be seamless.
Systems should comply with DICOM for imaging and HL7 for data exchange. This ensures compatibility with referrers’ practice software and hospital systems.
Referrers increasingly expect online portals rather than fax or email. Secure web access speeds reporting and strengthens referral relationships.
Teleradiology workflows allow after-hours coverage. This requires careful configuration of secure VPN access and RIS permissions. AI support is emerging but must be TGA-approved before clinical use.
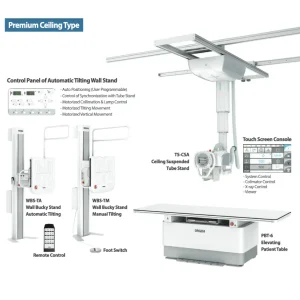
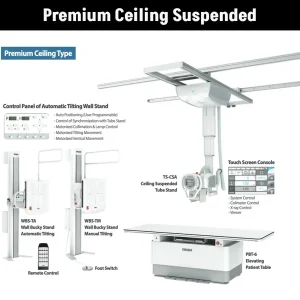
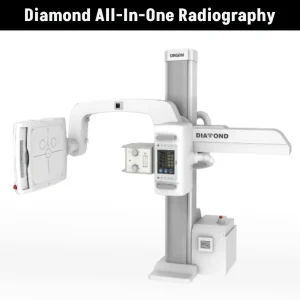
Our X-ray range
Our X-ray range options for your clinic.
7. Compliance and Quality Assurance
Compliance is not just initial accreditation. It is ongoing.
All staff exposed to radiation must wear personal dosimeters, with results logged and reviewed. Dose audits track patient exposures and highlight anomalies.
Preventive maintenance must be scheduled for all modalities. This reduces downtime and ensures equipment performs within regulatory limits.
Annual compliance testing is mandatory. Independent testers verify shielding, output levels, and QA processes. Medic Cloud assists centres in maintaining these compliance schedules.
See our piece on Personal Dose Monitors in Radiology for more detail.
8. Staffing and Human Resources
Radiology is workforce-intensive. Centres need radiographers licensed by state regulators, sonographers accredited for ultrasound, and FRANZCR-qualified radiologists. Depending on modality mix, nurses may be required for interventional procedures.
Workforce challenges differ by geography. In metro areas, competition for staff is high. In rural settings, recruitment can take months. Rostering must cover extended hours and after-hours teleradiology.
Training cannot be ignored. Staff must be trained not just on modalities but on IT systems, cybersecurity, and compliance protocols. OH&S and infection control are core obligations.
9. Financial and Insurance Considerations
Establishing a radiology centre is capital heavy. CT, MRI, and CBCT represent major investments. Business cases must balance capex against Medicare rebate income.
Opex models include managed ICT services, service contracts for modalities, and compliance costs. Medic Cloud does not lease hardware, so centres purchase modalities outright.
Insurance is essential. Specified item coverage generally proves more cost-effective than extended warranties. Policies must cover accidental damage, surges, fire, and flood. We’ve written about this in X-Ray System Accidental Insurance: Do I Need It?.
10. Project Timeline
A realistic build takes 12–18 months:
- Feasibility & Business Case (2–3 months) financial modelling, referral mapping.
- Design & Approvals (3–6 months) shielding plans, ARPANSA, council permits.
- Fit-Out & Infrastructure (6–9 months) building works, cabling, HVAC, shielding installation.
- Procurement & Installation (3–6 months) modalities, servers, workstations.
- Integration & Testing (1–2 months) RIS/PACS setup, security checks.
- Compliance Sign-Off (1–2 months) accreditation testing, DIAS submission.
- Go-Live & Training (4–6 weeks) staff induction, workflows, referrer onboarding.
Delays occur when coordination fails. Medic Cloud reduces this risk by managing all moving parts under one plan.
11. How Medic Cloud Delivers
Medic Cloud is unique in combining ICT expertise with diagnostic imaging specialisation. We manage projects end-to-end, providing a single point of accountability.
Our role includes:
- Coordinating builders, shielding consultants, and vendors
- Supplying and configuring servers, networks, printers, and workstations
- Installing and supporting imaging modalities (X-ray, CT, CBCT, DEXA, Ultrasound, Mammography, OPG/CEPH)
- Delivering RANZCR-compliant reporting stations
- Providing ongoing managed ICT services to keep centres compliant, secure, and scalable
We hope you have found our Radiology Centre Setup Guide useful. By partnering with Medic Cloud, your centre is designed, built, and operated correctly from day one.
For more information read the FAQS about setting up a clinic or contact us today for a conversation.
Read more blogs

Subscribe to Medic Hub
Get the latest insights direct to your inbox.